Discover practical insights for effective leadership in medical training with a focus on key concepts like the SMARTER model, team management styles, and situational leadership. Our guide discusses the importance of self-reflection, pacing in leadership, and applying a model based on environment, behaviour, beliefs, values, identity, and vision. Emphasizing collaboration, innovation, and excellence in the dynamic field of medical training, the guide outlines a commitment to empowerment and transformative leadership. Exploring leadership styles, it concludes with an overview of directing, coaching, supporting, and delegating, offering detailed behavioural approaches. A valuable resource for healthcare professionals navigating the complexities of leadership in medical training.
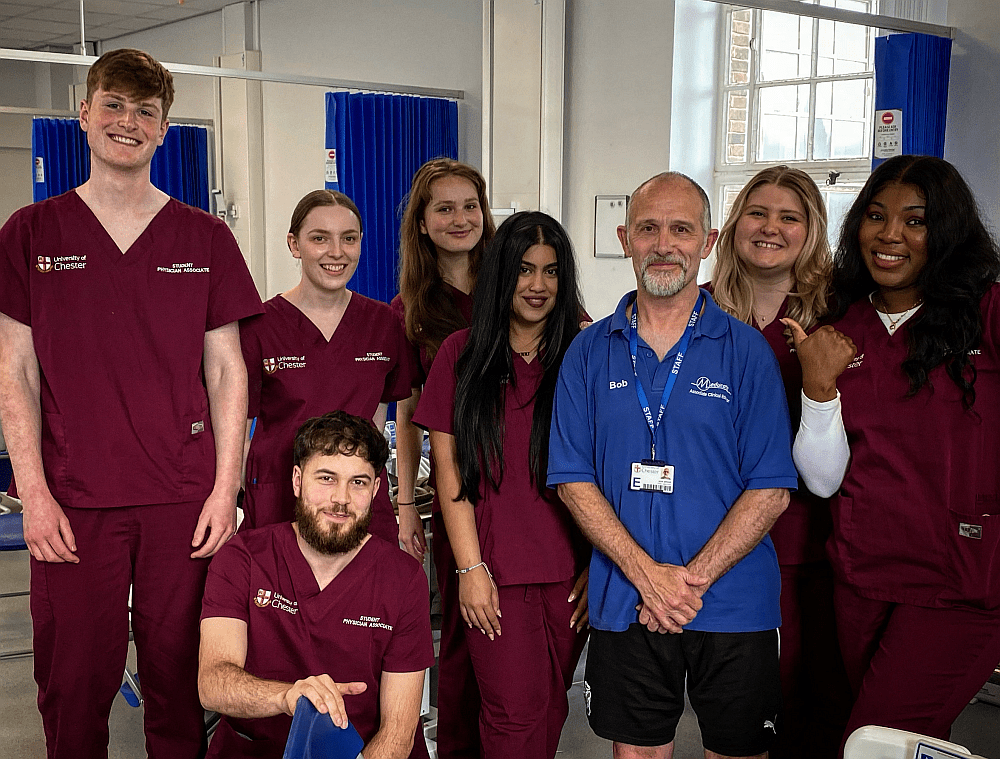
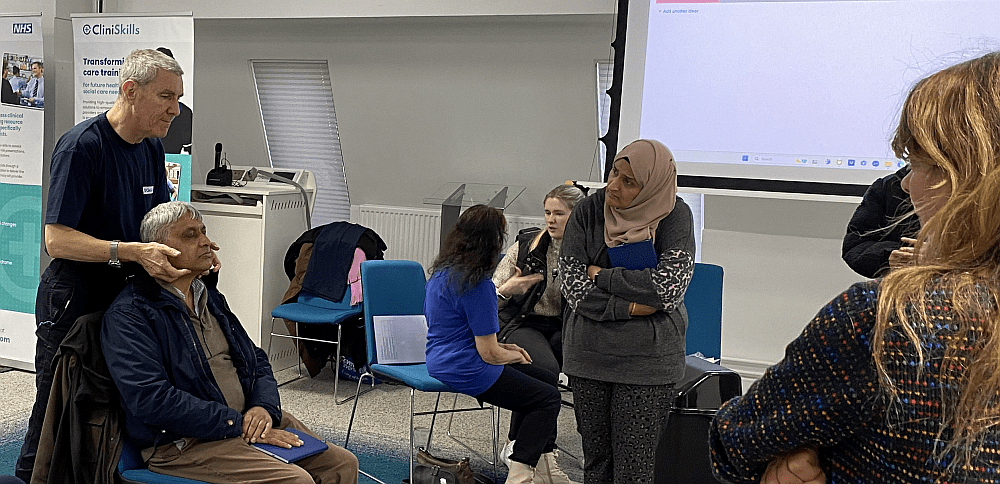
In my extensive experience collaborating with various organizations and overseeing my personal ventures, such as managing one of the largest Muay Thai groups in the UK and founding the Meducate Academy, I’ve come to understand the essence of effective leadership. Leading from the front, actively participating, and providing support are pivotal elements in successful leadership—a stark contrast to organizations merely paying lip service to teamwork.
Frustration often arose when working for teams that didn’t align actions with their words. This discontent led me to prefer entrepreneurial pursuits, where I could both work for myself and empower others. Many have asked me about the qualities of a good leader, prompting me to reflect on and document my fundamental leadership principles.
Here’s a concise overview of key ideas I apply daily. Your insights and experiences on these concepts are highly encouraged:
“When the best leader’s work is done, people say, ‘We did it ourselves’.”
Embrace the SMARTER Model:
· Specific
· Measurable
· Achievable
· Realistic
· Timely
· Ecology
· Resources
Recognize the 4 team management styles, with the ultimate aim of becoming a situational leader:
· A boss has conscripts; a leader has recruits.
· A boss wields power; a leader holds influence.
· A boss says “I will”; a leader says “we will.”
· A boss gets people to do things; a leader inspires them to want to do things.
· A boss is obeyed; a leader is followed.
Reflect on your leadership role in life:
· Identify existing leadership roles.
· Consider where you serve as a role model.
· Define what aspect of leadership appeals to you.
· Explore why you want to be a leader and what it will bring you.
Understand the importance of pacing in leadership, acknowledging and aligning with others’ starting points.
Pacing in Organizations Leading in Organizations:
· Manager – Leader
o Seeks control. – Facilitates change
o Keeps procedures going. – Creates new procedures
o Does things right. – Does the right things
o Mainly at the neurological level of skill. – At the neurological level of identity
o Administration. – Innovation
o Get people to do things. – Get people to want to do things by appealing to their beliefs and identity
When thinking about leadership and team building I tend toward using the following model:
ENVIRONMENT
Current Circumstances: Engaged in the dynamic field of medical training, navigating the challenges and opportunities that arise within this evolving landscape.
Workplace Details and Colleagues: Collaborating with a diverse team of healthcare professionals, educators, and administrators. Thriving in an environment that values innovation, teamwork, and excellence in medical education.
Daily Routine and Impact on Others: Diligently shaping the medical training landscape. My contributions positively impact colleagues by fostering a culture of continuous learning, effective collaboration, and patient-centred care.
BEHAVIOR AND CAPABILITIES
Skills and Appreciated Qualities: Demonstrate proficiency in your relevant skills, with a keen ability to specialise.
Recognized Strengths and Praised Attributes: Acknowledged for Specific Strengths, including Strategic Planning, and Decision-making. Colleagues appreciate my Attributes, e.g., empathy that enhances team dynamics and elevates the workplace culture.
Communication Skills: Possess strong verbal and written communication skills, effectively conveying complex medical concepts to diverse audiences. Recognized for fostering open communication and active listening within the team.
BELIEFS AND VALUES
Importance of Leadership: Hold a deep conviction regarding the transformative power of leadership in advancing medical training and healthcare. Believe that strong leadership is instrumental in creating a positive impact on both professionals and patient outcomes.
Desired Accomplishments: Aspire to your Leadership Goals, e.g., enhance medical curriculum, and foster interdisciplinary collaboration to contribute significantly to the advancement of medical education. Committed to achieving tangible outcomes that reflect excellence and innovation.
Beliefs About Good Leadership: Adhere to the philosophy that good leadership involves your Leadership Philosophy, e.g., empowering others, leading by example. Value collaborative decision-making, inclusivity, and a visionary approach to navigating challenges in the medical field.
IDENTITY
Self-Perception as a Leader: Embrace my role as a leader with humility, recognizing the privilege and responsibility it entails. Strive to be an authentic, approachable leader who leads with integrity and empathy.
Alignment with Personal Values and Lifestyle: Align leadership practices with your values, e.g., integrity, and continuous learning. Integrate leadership seamlessly into your lifestyle, emphasizing the importance of a balanced and purposeful approach.
Preferred Leadership Models: Draw inspiration from leadership models that prioritize your Preferred Leadership Models, e.g., servant leadership, and transformational leadership. Continuously seek to evolve and refine your leadership style to meet the evolving needs of the medical training landscape.
VISION
Motivations for Leadership: Motivated by the opportunity to contribute to the future of healthcare through impactful leadership in medical training. Aspire to inspire and nurture the next generation of healthcare professionals.
Vision Fuel Sources: Driven by a vision fueled by:
· Personal development: Constantly evolving as a leader and learner.
· Relationships: Building strong, collaborative partnerships within and beyond the medical community.
· Family: Striving for a healthcare system that prioritizes the well-being of families and communities.
· Work: Envisioning a workplace that values innovation, inclusivity, and continuous improvement.
· Health: Committed to promoting health and wellness within the medical community.
· Leisure: Finding inspiration and rejuvenation in moments of leisure to sustain passion and commitment.
This leadership CV encapsulates a commitment to mastering leadership within the intricate realm of medical training, emphasizing collaboration, empowerment, and a transformative approach to leadership.
Exploring Leadership Styles and Behaviours
1. Directing: Providing Specific Instructions and Close Supervision
In the directing leadership style, a leader takes charge by offering precise instructions and closely overseeing tasks. This approach is often employed in situations where clarity and control are paramount. A directing leader provides a roadmap for team members, leaving little room for interpretation. This style is effective in high-stakes scenarios where immediate decisions and actions are crucial.
Behavioural Approach: Directive
· Structure: Clearly outline tasks, goals, and expectations.
· Supervise: Monitor progress closely, ensuring adherence to guidelines.
· Control: Establish a controlled environment, maintaining order and discipline.
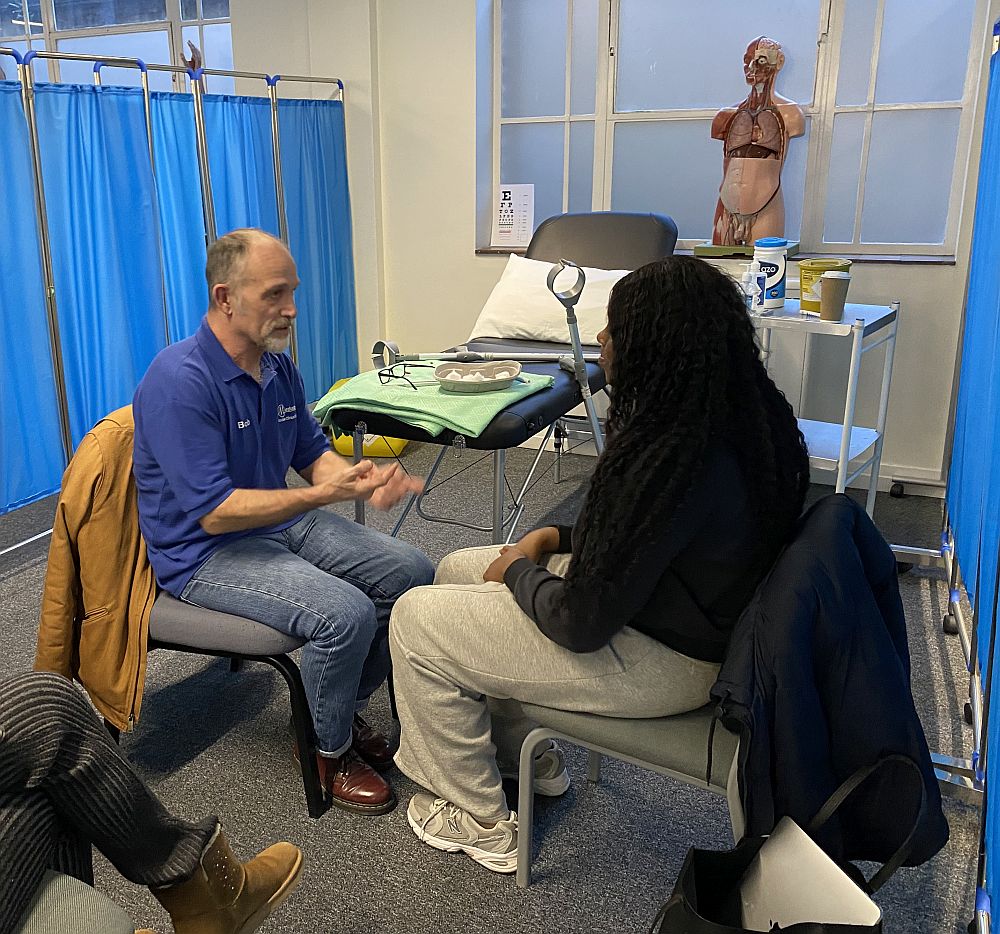
2. Coaching: Directing, Supervising, Explaining, Soliciting Suggestions, and Supporting Progress
Coaching involves a more interactive leadership style, where the leader not only provides guidance but actively engages with team members. This approach includes explaining decisions, seeking input, and offering support for personal and professional growth. The coaching style is effective in developing team members’ skills and fostering a collaborative environment.
Behavioural Approach: Directive and Supportive
· Structure: Provide a framework while encouraging input.
· Supervise: Offer guidance and support, ensuring progress.
· Listen: Actively engage with team members, seeking and valuing their input.
· Encourage: Support individual and team progress, praising achievements.
3. Supporting: Facilitating and Supporting Subordinates’ Efforts
The supporting leadership style involves empowering team members by offering guidance and facilitating their efforts. This approach values collaboration and shared responsibility for decision-making. Leaders who adopt this style create an environment where individuals feel supported and encouraged to contribute their ideas and skills.
Behavioural Approach: Supportive
· Praise: Acknowledge and appreciate team members’ contributions.
· Facilitate: Enable collaboration and provide necessary resources.
· Listen: Foster open communication, valuing diverse perspectives.
· Encourage: Cultivate a supportive atmosphere, promoting shared responsibility.
4. Delegating: Turning Over Responsibility and Problem-Solving
Delegating is a leadership style where the leader entrusts team members with responsibilities and problem-solving tasks. This approach relies on the expertise and autonomy of team members, promoting a sense of ownership. Leaders who adopt a delegating style empower their team to take initiative and showcase their skills.
Behavioural Approach: Supportive
· Praise: Recognize achievements resulting from delegated responsibilities.
· Facilitate: Ensure team members have the necessary resources and support.
· Listen: Encourage open communication for effective problem-solving.
· Encourage: Reinforce a culture of initiative and autonomy.
Avoiding Seagull Management: Consistent Commitment and Engagement
Seagull management, characterized by swooping in, creating chaos, and departing, is detrimental to effective leadership. Leaders should steer clear of this approach and instead focus on consistent commitment and engagement. Effective leadership requires ongoing dedication to understanding team dynamics, fostering a positive work environment, and providing continuous support. By avoiding the pitfalls of seagull management, leaders can establish trust, build strong teams, and achieve sustained success in their endeavours.
If you’re a Clinical Lead and wish to discuss working with Meducate Academy Ltd., we would love to give you a demonstration and a workshop at your institution.
Please contact: bobspour@meducateacademy.com or on 07870 611850