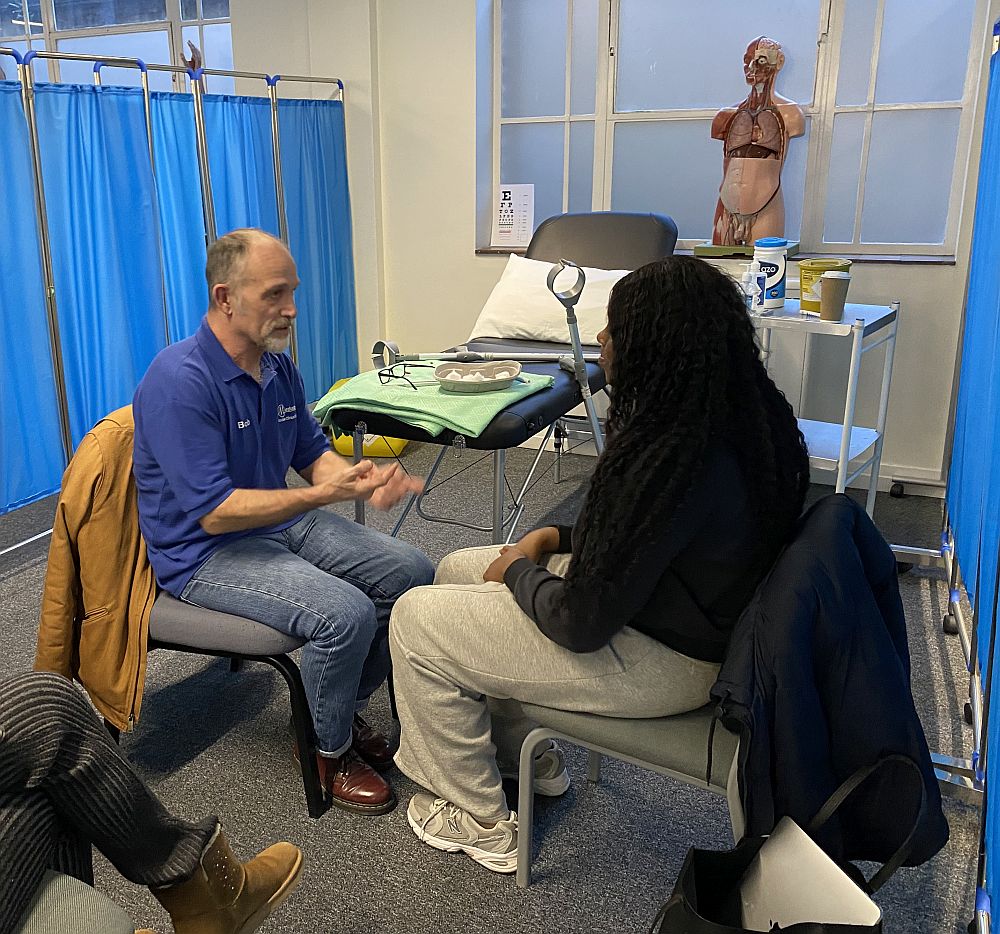
Meducate Academy Founder and Training Director Bob helps a Pharmacy Undergraduate deal with a difficult patient
Navigating the intricacies of clinical communication is imperative for Associate Clinical Educators as they mould the next generation of healthcare professionals. Understanding this necessity, I’ve meticulously crafted a condensed yet thorough resource to bolster teaching efforts. Whether guiding budding medical practitioners or refining personal aptitude, this guide is designed to serve as an invaluable asset.

Associate Clinical Educator Mike Kinsella explains the importance of good communication with Undergraduate Pharmacists at The University of Birmingham
As an Associate Clinical Educator, it’s crucial for us to periodically revisit the expectations we have for our students concerning clinical communication. Recognizing this need, I’ve developed a concise yet comprehensive aid to assist you during your teaching endeavours. Whether you’re guiding aspiring medical professionals or refreshing your understanding, this simplified aide memoire aims to be a valuable resource for all.
In the realm of medicine, effective communication is not just a skill; it’s an art form. From conveying critical information to patients and their families to collaborating seamlessly with colleagues, the ability to communicate clearly and empathetically is paramount for any healthcare professional. In this guide, we delve into the importance of clinical communication for healthcare providers and offer valuable insights to help master this essential aspect of medical practice.
Why is Clinical Communication Important?
Clear and effective communication lies at the heart of quality healthcare delivery for several reasons:
1. Patient Understanding: Patients often come to healthcare settings feeling vulnerable and anxious. Clear communication helps them understand their condition, treatment options, and what to expect, fostering trust and cooperation.
2. Informed Decision-Making: Informed consent is a cornerstone of medical ethics. Effective communication ensures that patients have the information they need to make decisions about their care that align with their values and preferences.
3. Team Collaboration: Healthcare is rarely a solitary endeavour. Effective communication among healthcare teams is crucial for coordinated care, preventing errors, and optimizing patient outcomes.
4. Empathy and Support: Patients and their families are not just cases; they are human beings facing challenging circumstances. Empathetic communication can provide comfort and support, improving the overall patient experience.
Key Principles of Clinical Communication
1. Active Listening: This involves not just hearing, but truly understanding what the patient is saying. Pay attention to both verbal and nonverbal cues, and encourage patients to express their concerns and preferences.
2. Clarity and Simplicity: Medical jargon can be confusing for patients. Use plain language and avoid technical terms whenever possible. Ensure that patients leave consultations with a clear understanding of their condition and treatment plan.
3. Empathy and Respect: Treat patients with dignity and respect, and strive to understand their perspectives and emotions. Empathy goes a long way in building trust and rapport.
4. Cultural Competence: Recognize and respect cultural differences that may influence communication preferences and healthcare decisions. Tailor your approach accordingly to ensure effective communication across diverse patient populations.
5. Nonverbal Communication: Body language, facial expressions, and tone of voice can convey as much meaning as words. Maintain eye contact, use open body language, and convey warmth and compassion in your interactions.
6. Adaptability: Every patient is unique, and what works for one may not work for another. Be flexible in your communication style, adapting it to suit the individual needs and preferences of each patient.
Tools and Techniques for Improving Clinical Communication
1. Patient-Centered Communication Models: Familiarize yourself with frameworks such as the SPIKES protocol for breaking bad news or the teach-back method for confirming patient understanding. These structured approaches can help streamline communication and ensure key points are addressed.
2. Role-Playing and Simulation: Practice communication skills through role-playing exercises or simulation scenarios. This allows you to hone your abilities in a safe and supportive environment, receiving feedback from peers and mentors.
3. Continuing Education: Attend workshops, seminars, and online courses focused on communication skills in healthcare. Continuing education opportunities can provide valuable insights and strategies for enhancing your clinical communication abilities.
4. Feedback and Reflection: Solicit feedback from patients, colleagues, and supervisors on your communication skills. Reflect on your experiences, identifying areas for improvement and setting goals for ongoing development.
Conclusion
Effective clinical communication is not just a desirable skill; it’s an ethical imperative and a cornerstone of quality healthcare delivery. By embracing principles of empathy, clarity, and cultural competence, healthcare providers can forge stronger connections with patients, facilitate informed decision-making, and ultimately improve patient outcomes. Through ongoing practice, education, and reflection, mastering the art of clinical communication is within reach for every healthcare professional.
Join us on our journey of advancing healthcare education and empowering professionals for the challenges that lie ahead. Stay updated on our upcoming training sessions and university collaborations by bookmarking and following our blog Associate Clinical Educators.
If you’re a Clinical Lead or Medical Role Player and wish to discuss working with Meducate Academy Ltd., or if you would like us to give you a demonstration and a workshop at your institution.
Please contact: bobspour@meducateacademy.com or on 07870 611850