In medical education, the term “patient journey” refers to the comprehensive pathway a patient experiences from the onset of symptoms to the resolution of their health issue. This concept includes all interactions and processes a patient undergoes within the healthcare system. Here’s a detailed breakdown of the key aspects and how an Associate Clinical Educator (a highly trained Simulated Patient) can improve outcomes through high-fidelity simulation and feedback.
1. Initial Encounter
The initial encounter marks the beginning of the patient’s journey and includes the patient’s first recognition of symptoms and their initial steps to seek medical help. This phase can vary greatly depending on the individual’s health literacy, access to care, and socio-economic background. Patients may initially attempt self-care based on their understanding and available resources, seek advice from family or friends, or visit a primary care provider. This phase is crucial as it sets the tone for the subsequent healthcare experiences. In medical education, understanding this initial phase helps future healthcare professionals recognize the diverse entry points into the healthcare system and the barriers patients may face in accessing care.
Health Literacy and Socio-economic Factors
Health literacy plays a significant role in how patients recognize symptoms and decide on their initial steps. Those with higher health literacy are more likely to identify symptoms accurately and seek appropriate care promptly. Socio-economic factors, such as income, education, and access to healthcare services, also influence this initial encounter. For example, individuals from lower socio-economic backgrounds may delay seeking medical help due to financial constraints or lack of nearby healthcare facilities.
Barriers to Access
Recognizing and understanding the barriers patients face in accessing care is essential for medical professionals. These barriers can include geographic limitations, financial issues, cultural beliefs, and previous negative experiences with the healthcare system. Addressing these barriers is crucial for improving patient outcomes and ensuring equitable access to healthcare.
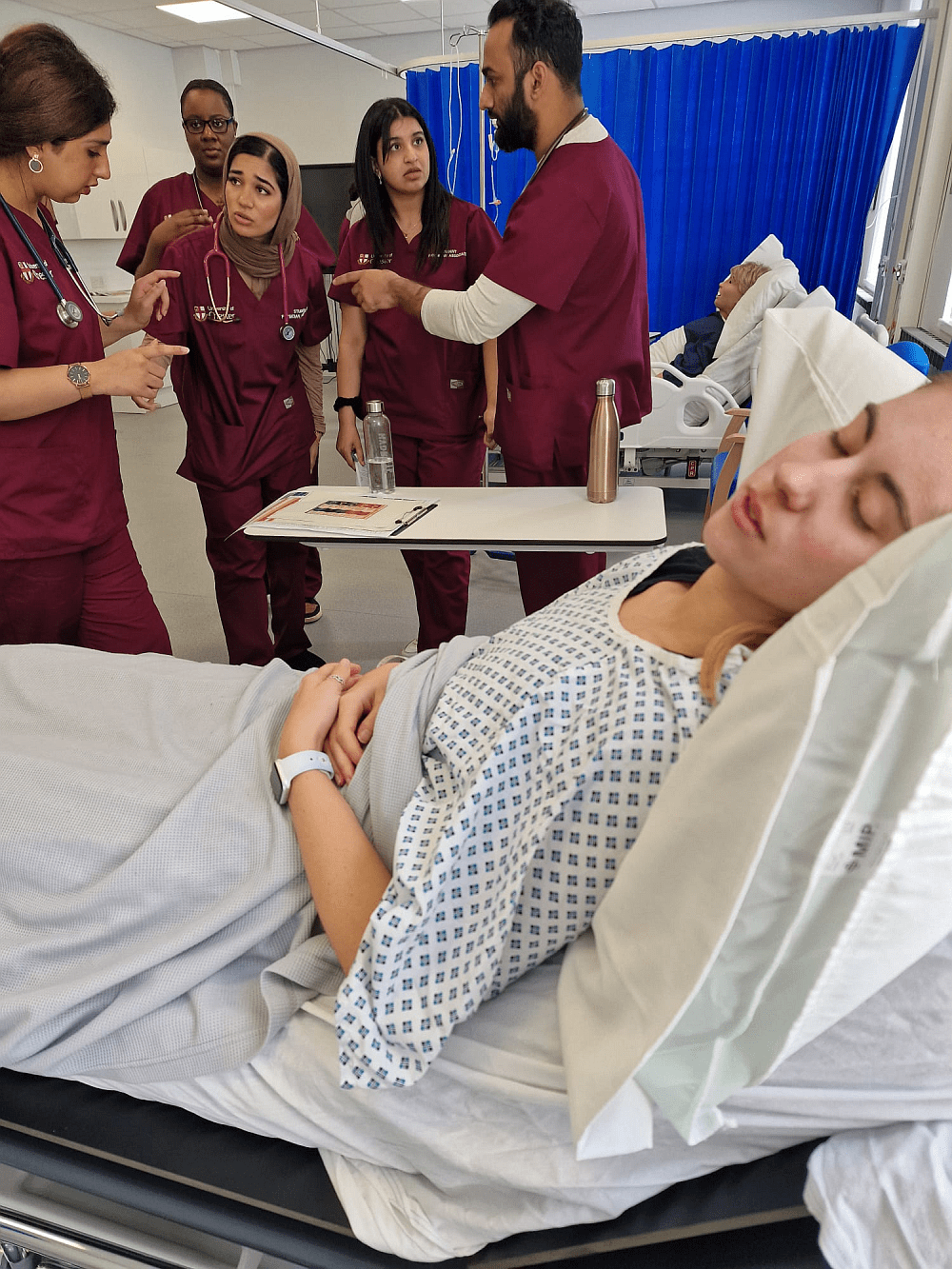
Role of the Associate Clinical Educators
ACEs play a crucial role in medical education, particularly in training students to handle initial patient encounters effectively. They are highly trained lay educators & in most cases trained roleplayers who portray patients with specific medical conditions and backgrounds, allowing students to practice and refine their communication and clinical skills in a controlled, realistic setting.
– Enhanced Communication Skills: ACEs provide students with the opportunity to practice eliciting patient histories, understanding patient concerns, and explaining medical concepts in a way that is understandable to individuals with varying levels of health literacy.
– Cultural Competence: ACEs can be used to represent diverse socio-economic and cultural backgrounds, helping students develop cultural competence and learn how to address potential biases and barriers to care.
– Immediate Feedback: ACEs can give immediate, structured feedback from the patient’s perspective, helping students improve their bedside manner, empathy, and ability to make patients feel heard and respected.
– Scenario Variety: Through ACE encounters, students are exposed to a wide range of initial presentation scenarios, from common physical & psychological symptoms to rare conditions, helping them build a broad base of experience and confidence.
– Safe Learning Environment: Using ACEs allows students to make mistakes and learn from them without causing harm to real patients, fostering a safer learning environment and encouraging a growth mindset.
2. Diagnosis
The diagnostic process is a critical step where healthcare professionals gather the patient’s medical history, perform physical examinations, and order diagnostic tests to identify the underlying cause of the symptoms. This phase involves clinical reasoning and decision-making skills, which are fundamental components of medical training. The accuracy and efficiency of the diagnostic process directly impact the patient’s subsequent treatment and outcomes. Medical students and trainees learn the importance of taking a thorough history, conducting a detailed physical exam, and selecting appropriate diagnostic tests. Additionally, they are taught to consider differential diagnoses and to communicate findings effectively with patients and the healthcare team.
Role of Associate Clinical Educator
ACEs can significantly enhance the training during the diagnostic process:
– Clinical Reasoning: Students practice diagnostic reasoning with ACEs, learning to synthesise patient information and develop differential diagnoses.
– Examination Skills: ACEs help students refine their physical examination techniques and adapt their approach based on patient feedback.
– Diagnostic Tests Interpretation: Through ACE scenarios, students learn to select and interpret appropriate diagnostic tests, understanding the implications of their choices.
3. Treatment Planning
Once a diagnosis is made, developing a treatment plan is the next step in the patient journey. This plan may include medications, surgical interventions, lifestyle changes, or other therapeutic measures. Involving the patient and their family in this process is essential for ensuring that the treatment plan is realistic, acceptable, and adheres to the patient’s preferences and values. In medical education, emphasis is placed on shared decision-making and patient-centred care. Trainees learn to discuss the risks, benefits, and alternatives of treatment options with patients, considering their unique circumstances and goals. This phase highlights the importance of clear communication and the need for healthcare providers to be compassionate and empathetic.
Role of Associate Clinical Educator
ACEs enhance the development of treatment planning skills:
– Shared Decision-Making: ACEs allow students to practice engaging patients in treatment planning, considering their preferences and values.
– Communication of Risks and Benefits: Students learn to clearly explain treatment options, potential outcomes, and risks to patients.
– Patient-Centered Approach: Training with ACEs emphasizes the importance of empathy and respect in developing a collaborative treatment plan.
4. Treatment and Management
The treatment and management phase involves implementing the treatment plan. Patients may need to visit various healthcare providers, undergo procedures, or adhere to specific medication regimens. This phase often requires coordination among multiple healthcare professionals, including specialists, nurses, and allied health staff. Medical education programs stress the importance of interdisciplinary teamwork and the role of each team member in providing comprehensive care. Students are trained in care coordination, time management, and the use of healthcare technologies that facilitate communication and collaboration. This phase also includes managing potential complications and adjusting the treatment plan as necessary based on the patient’s response.
Role of Associate Clinical Educator
ACEs contribute to improving treatment and management skills:
– Interdisciplinary Collaboration: ACE scenarios often involve multiple healthcare providers, teaching students how to work effectively in teams.
– Care Coordination: Students practice coordinating care among different providers and settings, ensuring comprehensive management of the patient’s condition.
– Adaptability: ACEs help students learn to adjust treatment plans based on patient responses and emerging complications.
5. Follow-up and Monitoring
After the initial treatment, ongoing follow-up is necessary to monitor the patient’s progress, manage any side effects, and make adjustments to the treatment plan as needed. Regular follow-up appointments, lab tests, and imaging studies may be part of this phase. It ensures that the patient is recovering well and that any complications are promptly addressed. In medical education, this phase emphasizes the importance of continuity of care and the role of primary care providers in maintaining long-term patient relationships. Trainees learn to develop follow-up plans, recognize early signs of complications, and provide ongoing support to patients as they navigate their health journey.
Role of Associate Clinical Educator
ACEs play a vital role in training for follow-up and monitoring:
– Long-Term Relationships: Students practice maintaining ongoing relationships with ACEs, simulating real-world follow-up scenarios.
– Monitoring and Adjusting Care: ACEs help students learn to monitor patient progress and make necessary adjustments to the treatment plan.
– Recognition of Complications: Through ACE interactions, students develop the skills to identify and address potential complications early.
6. Outcome and Long-term Care
The patient journey also encompasses long-term outcomes and any necessary chronic care management. This could involve rehabilitation, ongoing medication, lifestyle adjustments, or palliative care in some cases. Long-term care aims to maintain or improve the patient’s quality of life and manage any chronic conditions effectively. Medical education programs highlight the importance of chronic disease management, rehabilitation medicine, and palliative care. Students are taught to develop long-term care plans, coordinate with other healthcare providers, and support patients and their families in managing ongoing health issues. This phase underscores the need for a holistic approach to patient care that addresses physical, emotional, and social aspects of health.
Role of Associate Clinical Educator
ACEs improve training in long-term care and outcomes:
– Chronic Disease Management: ACEs simulate patients with chronic conditions, allowing students to practice developing and managing long-term care plans.
– Rehabilitation and Palliative Care: Students engage with ACEs to understand the complexities of rehabilitation and end-of-life care.
– Holistic Care: ACEs help students appreciate the importance of addressing physical, emotional, and social needs in long-term care.
7. Patient Experience
Throughout the patient journey, the patient’s experience is a crucial component. This includes their interactions with healthcare providers, the clarity of information provided, emotional support, and overall satisfaction with the care received. Patient experience directly impacts health outcomes and adherence to treatment plans. In medical education, understanding the patient experience is essential for training healthcare professionals to provide compassionate and empathetic care. Trainees learn to listen actively to patients, address their concerns, and ensure they feel valued and respected throughout their healthcare journey. Programs often incorporate patient feedback and case studies to highlight the importance of patient-centred care and continuous quality improvement.
Role of Associate Clinical Educator
ACEs significantly enhance the understanding and improvement of patient experience:
– Empathy and Compassion: ACEs provide feedback on students’ communication and interpersonal skills, fostering empathy and compassion.
– Active Listening: Students practice active listening with ACEs, learning to address patient concerns effectively.
– Patient Satisfaction: Training with ACEs helps students understand the factors that contribute to patient satisfaction and overall experience.
Understanding the patient journey in medical education is essential for training healthcare professionals to provide holistic and patient-centered care. It helps students and practitioners appreciate the importance of each step in the process and the need for effective communication, empathy and coordination among healthcare providers to ensure the best outcomes for patients. By comprehensively understanding the patient journey and incorporating ACEs into training, future healthcare professionals can enhance the quality of care and improve the overall patient experience.
Transform Your Healthcare Training with Meducate Academy
- Are you an institution or training organization providing healthcare education for Medical Students, Physician Associates, Nurses, Pharmacists, or Physiotherapists?
- Do you incorporate simulation as part of your teaching methodology?
- Do you aspire for your students to excel in medical knowledge, communication skills, and safe practice?
If you answered yes to any of these questions, Meducate Academy will elevate your training programs. With over 25 years of experience, our Associate Clinical Educators specialize in advanced simulation techniques to enhance your curriculum.
We have successfully delivered training courses for Physician Associates, Medical Students, Pharmacists, and Nurses. Recently, we have been honoured to collaborate with The Royal Orthopaedic Hospital in Birmingham, assisting in the teaching of musculoskeletal examinations to 3rd and 4th-year medical students from the University of Birmingham and Aston University.
Our impressive clientele includes the University of Birmingham (Pharmacy), the University of Newcastle, the University of Chester (Physician Associate students), and the University of Wolverhampton (Pharmacists). Additionally, we are proud educational partners of The Pharmacy Show, held annually at the NEC, collaborating with our partners at Cliniskills.
We are excited to introduce our latest educational package, “The Patient Journey – A Hands-On Approach”. We invite organizations to join us in this innovative training experience and help shape the future of healthcare education.
Contact Meducate Academy today to take your training programs to the next level.
For an informal chat please get in touch with me: bobspour@meducateacademy.com or on 07870 611850











 Once the weekend was over we were booked to work with 2nd year PAs at the Riverside Campus at the University of Chester. They tasked us with delivering a whole range of skills. We went through all the systems exams from Musculo-skeletal, through Cardiovascular examinations and some challenging scenarios thrown in. One of our team also ran a breast examination station, giving the students an opportunity to practice important but often neglected skills, including feedback on their technique from the associate clinical educator.
Once the weekend was over we were booked to work with 2nd year PAs at the Riverside Campus at the University of Chester. They tasked us with delivering a whole range of skills. We went through all the systems exams from Musculo-skeletal, through Cardiovascular examinations and some challenging scenarios thrown in. One of our team also ran a breast examination station, giving the students an opportunity to practice important but often neglected skills, including feedback on their technique from the associate clinical educator.