
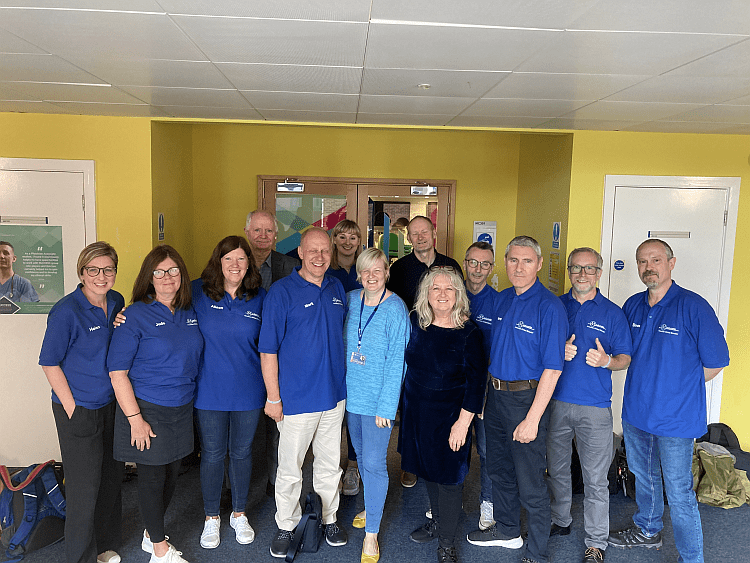
Being an Associate Clinical Educator (ACE) is a rewarding and dynamic role that contributes to the education and growth of future healthcare professionals. The ACEs receive immense fulfilment from positive student feedback and witnessing their progress. The job brings excitement and unpredictability, requiring adaptability and improvisation to deliver effective educational content. ACEs gain valuable experience from working with diverse clinicians, undergo regular training and evaluation to stay updated, and ensure the quality of education. Recently, at Newcastle University Medical School, a four-person ACE team provided comprehensive MSK examination training and extended support in other areas of healthcare education. The students appreciated learning from experienced ACEs and requested guidance on various exams. Despite time constraints, consultation skills were briefly covered, and a group Q&A session concluded the day. Gratitude was expressed to the university staff for their collaboration in creating a valuable learning environment.

Working as an Associate Clinical Educator (ACE) is an incredibly fulfilling and stimulating role. ACEs play a vital role in the education and development of future healthcare professionals, and the rewards of this position are often experienced on a personal and professional level. The positive feedback received from students after a job well done is a source of immense fulfilment. Knowing that your efforts have contributed to their growth and progress is a testament to the significance of the ACE role.
One aspect that makes this role exciting is the unpredictability it brings. The subject matter can change at a moment’s notice, from cranial nerves to a cardio examination with a roleplay element added spontaneously. These unexpected twists and turns add an element of excitement and keep the role fresh and invigorating. As ACEs, it is crucial to be adaptable and ready to improvise, as this flexibility ensures the effective delivery of educational content.
The ability to adapt and improvise stems from the wealth of experience ACEs gain from working with clinicians from diverse backgrounds. This experience equips them with the necessary skills and knowledge to handle various teaching scenarios. To ensure the continuous professional development of ACEs, regular training sessions and a rigorous evaluation process are implemented. These measures not only guarantee that ACEs are up to date with the latest advancements but also uphold the quality of education they provide.
Recently, at Newcastle University Medical School, we had the privilege of teaching MSK examinations to 2nd Year Physician Associate students. Musculoskeletal (MSK) is one of our specialties, and our expertise in this field is derived from training with renowned clinicians and collaborating with members of the FRCS. Our knowledge is cutting-edge, ensuring that students receive the most up-to-date information.

The positive feedback we received from our previous visit to Newcastle prompted the university to invite us back for further training. While the students initially exhibited some reticence, having only practiced on each other, our four-person ACE team quickly alleviated their fears. The advantage of having a small student-to-ACE ratio allowed us to delve into details and answer their questions promptly and effectively. We covered a range of MSK examinations, including the hip, knee, shoulder, and spine. Additionally, we fulfilled requests for hand and ankle exams, ensuring a comprehensive learning experience. Our instruction included all the special tests for MSK, providing continuous feedback to aid their learning. The students greatly appreciated the opportunity to learn from experienced ACEs rather than relying solely on practicing with their peers. One student even humorously remarked that it was a case of the blind leading the blind!
Surprisingly, some students were amazed at our level of knowledge of other body systems. They requested that we check their cardio, GI, and respiratory exams ahead of their upcoming OSCEs (Objective Structured Clinical Examinations). As ACEs, our expertise extends beyond our specialization, allowing us to provide guidance and support in various areas of healthcare education.
Although time constraints prevented us from fully exploring consultation skills, we provided the students with a brief overview of the basics. We reassured them that their history-taking skills were up to par for their current stage of training.
As the day came to an end, we conducted a group Q&A session to address any remaining questions. We expressed our gratitude to the students for their active participation and made the journey back to Birmingham, reflecting on the meaningful interactions and knowledge shared.
We would like to extend our heartfelt thanks to Alice Fitzpatrick, Year 2 & EDI Lead for MSc Physician Associate Studies, and Emma McAllister, Degree Program Director, MSc Physician Associate Studies, for granting us the opportunity to teach at Newcastle University. Their support and collaboration have been instrumental in fostering a rich learning environment for the students.
In Other News…
Exciting times are ahead for Meducate Academy as we prepare to launch our latest offering: Pharma Pathways. This is a programme of training designed to support clinical pharmacists. In collaboration with experienced Clinical Lecturers in Clinical Pharmacy, we aim to assist pharmacists in meeting the new government directive regarding consultation and clinical skills training. Through our dedicated ACEs and Medical Roleplayers, who possess decades of experience working with healthcare professionals such as Physician Associates and Nurses, we are committed to delivering comprehensive support.
Currently, Meducate Academy supplies ACEs and Medical Roleplayers to pharmacy programs at both the University of Wolverhampton and Birmingham, further expanding our reach and impact in the field of healthcare education. Pharma Pathways has been created to offer educators access to ACEs and Medical Roleplayers.
In conclusion, the role of an Associate Clinical Educator is undeniably fulfilling, interesting, and exciting. It provides opportunities for personal growth and professional development while positively influencing the education and future careers of aspiring healthcare professionals.
If you’re a Pharmacy Clinical Lead and wish to discuss working with Meducate Academy Ltd., we would love to give you a demonstration and a workshop at your institution.
Please contact: bobspour@meducateacademy.com or on 07870 611850






 The ACE plays a very important part in this process, and because of their high level of knowledge and skill can replicate the patient journey in fine detail. This is what distinguishes us from volunteers or role-players, who give high-fidelity feedback on more than just communication skills. An Ace is trained to give feedback on the way a student handled the patient, and the efficacy of the techniques they are using. For example, the way the student auscultates and percusses the patient or the way the student used palpation.
The ACE plays a very important part in this process, and because of their high level of knowledge and skill can replicate the patient journey in fine detail. This is what distinguishes us from volunteers or role-players, who give high-fidelity feedback on more than just communication skills. An Ace is trained to give feedback on the way a student handled the patient, and the efficacy of the techniques they are using. For example, the way the student auscultates and percusses the patient or the way the student used palpation.







 The role of the ACE™ therefore is to give feedback on all of the above. This will ensure that the student performs the examination correctly,to the standard of the current OSCE curriculum and demonstrates safe practice. As you can see the function of the ACE™ far exceeds that of a simulated patient or role player.
The role of the ACE™ therefore is to give feedback on all of the above. This will ensure that the student performs the examination correctly,to the standard of the current OSCE curriculum and demonstrates safe practice. As you can see the function of the ACE™ far exceeds that of a simulated patient or role player.

