Meducate Academy – Reflecting on Our Recent Achievements and Future Goals in Medical Education
As summer approaches, it’s an ideal time to reflect on Meducate Academy’s accomplishments over the past few months and consider how we can continue to elevate our teaching standards. This period has been marked by a diverse array of topics and students, ranging from potential medical students to seasoned professionals, including pharmacists, physician associates, and doctors.
In this blog post, we’ll take a closer look at the busy months we’ve had at Chester University Medical School, our rewarding engagements with the Physician Associate Programme, and our collaborative efforts with Cliniskills. We’ll also share insights into our expanding reach to Aston and Kensington, ongoing work with the University of Birmingham Pharmacy undergraduates, and the exciting addition of Ruth Newton as our new Ambassador for Pharmacy. Stay tuned for upcoming events and more details on how we are continuously striving to make a meaningful impact in medical education.
Busy Months at Chester University Medical School
The University of Chester Medical School has kept us particularly busy, especially with the new medical school opening in September. Throughout April and May, we conducted numerous interviews to assess prospective students. It’s a privilege to be part of this process, focusing on evaluating candidates’ communication skills and problem-solving abilities. Alongside Mark Reynolds, who played the role of a patient during our roleplay sessions, I acted as an assessor, ensuring we identified students with strong interpersonal skills. While most sessions were held at the university, we also conducted several virtual interviews for international candidates on Teams.
Engaging Physician Associate Students
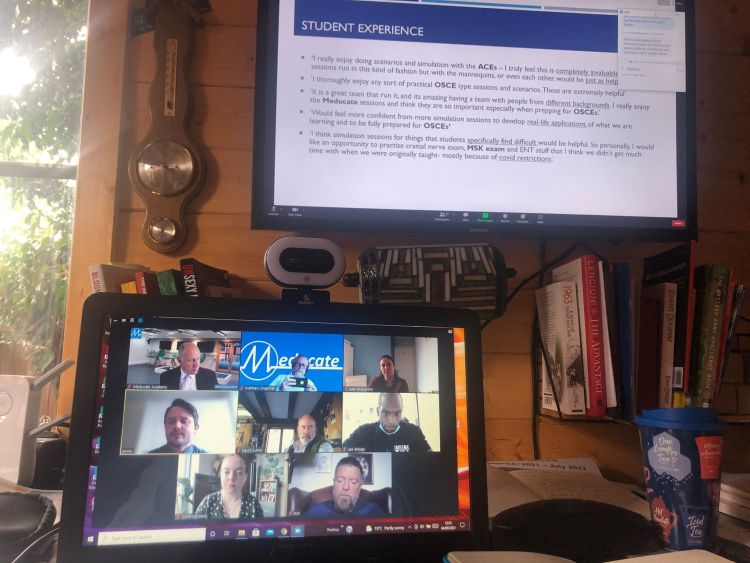
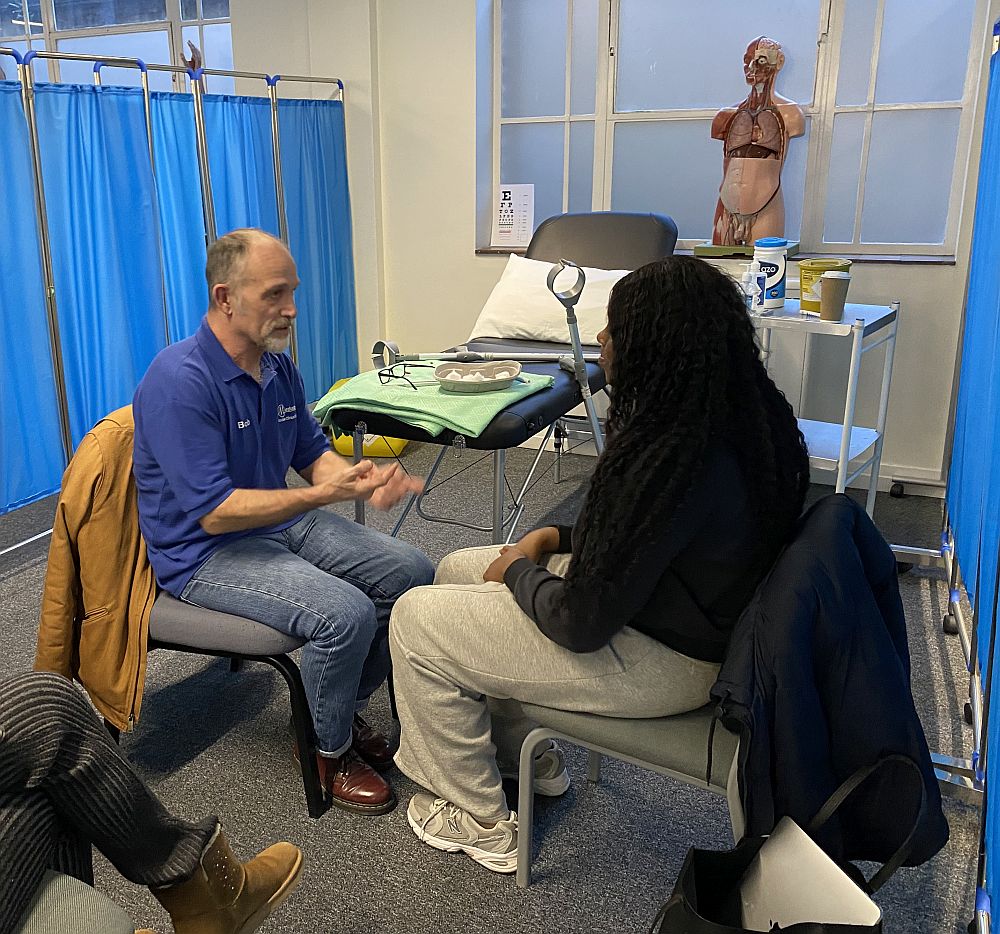
Our work with the Physician Associate Programme has been equally demanding and rewarding. We’ve primarily engaged with first-year students, helping them apply their foundational knowledge in cardiology, respiratory, gastrointestinal, and cranial nerve examinations. These sessions incorporated high-fidelity simulations to enhance their developing communication skills. The “Patient Journey” simulation, in particular, demonstrated the effectiveness of this blended learning approach.
In medical education, the term “patient journey” refers to the comprehensive pathway a patient experiences from the onset of symptoms to the resolution of their health issue. This concept includes all interactions and processes a patient undergoes within the healthcare system. Our ACEs provide the student Physician Associate with a realistic hi-fidelity simulation of a “real patient” Here’s a breakdown of the key aspects:
Initial Encounter: This includes the patient’s first recognition of symptoms and their initial steps to seek medical help, which could involve self-care, consulting with family, or visiting a primary care provider.
Diagnosis: The journey continues with the diagnostic process, where healthcare professionals gather the patient’s history, perform physical examinations, and order diagnostic tests to identify the underlying cause of the symptoms.
Treatment Planning: Once a diagnosis is made, a treatment plan is developed. This could involve medications, surgeries, lifestyle changes, or other therapeutic interventions. The plan may be discussed with the patient and their family, considering their preferences and concerns.
Treatment and Management: This phase includes the implementation of the treatment plan. The patient might need to visit various healthcare providers, undergo procedures, or follow specific regimens. This phase often requires coordination between multiple healthcare professionals.
Follow-up and Monitoring: After the initial treatment, ongoing follow-up is necessary to monitor the patient’s progress, manage any side effects, and make adjustments to the treatment plan as needed. This phase ensures that the patient is recovering well and that any complications are promptly addressed. (This would be discussed with the student but not simulated.)
Outcome and Long-term Care: The patient journey also encompasses the long-term outcomes and any necessary chronic care management. This could involve rehabilitation, ongoing medication, lifestyle adjustments, or palliative care in some cases.
Patient Experience: Throughout this journey, the patient’s experience is a crucial component. This includes their interactions with healthcare providers, the clarity of information provided, emotional support, and overall satisfaction with the care received. In this case, the ACE would give measured and accurate feedback on the process alongside a clinician who would give feedback on the clinical aspects of the interaction.
In medical education, understanding the patient journey is essential for training healthcare professionals to provide holistic and patient-centred care. It helps students and practitioners appreciate the importance of each step in the process and the need for effective communication, empathy, and coordination among healthcare providers to ensure the best outcomes for patients.
Collaborations with Salford University
In the Northwest, we had the opportunity to collaborate with the simulation team at Salford University. Greg and Mark delivered a comprehensive demonstration of musculoskeletal (MSK) examinations, both on-site and via Teams for remote participants. This experience highlighted our expertise in MSK examinations, an area where our founder and director, Bob, continues to make significant contributions at the Royal Orthopaedic Hospital in Birmingham as an independent ACE.
Expanding Our Reach: Aston and Kensington
Next, we expanded our reach to Aston and Kensington, working with a large team of Associate Clinical Educators (ACEs). In collaboration with Cliniskills, we ran several stations to teach pharmacists how to conduct ENT, cardiovascular, and blood pressure examinations. This was very well received and the work will continue into 2025.
Continuing with the theme of pharmacy, we also delivered training on gastrointestinal and respiratory examinations to experienced pharmacists at the Humanitarian Academy for Development. The pharmacists’ enthusiasm and engagement during these sessions were truly inspiring.
Ongoing Work with the University of Birmingham
Our ongoing collaboration with the University of Birmingham’s undergraduate pharmacy program has been highly productive. We have been actively involved in Objective Structured Clinical Examinations (OSCEs) and teaching sessions. In the coming weeks, we look forward to participating in staff training sessions.
Welcoming Ruth Newton and Upcoming Events
We are delighted to welcome Ruth Newton as our new Ambassador for Pharmacy. Ruth, a medical education and nutrition pharmacist at The Countess of Chester Hospital, also serves as a visiting lecturer for the Physician Associate Programme at the University. I’ll be hosting a podcast with Ruth for Meducate Academy soon, so stay tuned for that.
Additionally, we are excited to announce our involvement in this year’s Pharmacy Show at the NEC. Being invited once again as educational partners is an honour, and we look forward to bringing our workshops to a wider audience. More details on this will be shared soon.
In summary, the past few months have been a period of significant activity and achievement. As we move forward, we remain committed to improving our teaching standards and expanding our reach to make a meaningful impact in medical education.
Join us on our journey of advancing healthcare education and empowering professionals for the challenges that lie ahead. Stay updated on our upcoming training sessions and university collaborations by bookmarking and following our blog Associate Clinical Educators.
If you’re a Clinical Lead or Medical Role Player and wish to discuss working with Meducate Academy Ltd., or if you would like us to give you a demonstration and a workshop at your institution.
Please contact: bobspour@meducateacademy.com or on 07870 611850









 The Independent Prescribing Course is a medical education program designed to equip healthcare professionals with the necessary skills and knowledge to prescribe medication independently. This course is typically intended for healthcare professionals such as pharmacists, nurses, physiotherapists and optometrists who are required to prescribe medication as part of their professional responsibilities.
The Independent Prescribing Course is a medical education program designed to equip healthcare professionals with the necessary skills and knowledge to prescribe medication independently. This course is typically intended for healthcare professionals such as pharmacists, nurses, physiotherapists and optometrists who are required to prescribe medication as part of their professional responsibilities.
 The role of the ACE™ therefore is to give feedback on all of the above. This will ensure that the student performs the examination correctly,to the standard of the current OSCE curriculum and demonstrates safe practice. As you can see the function of the ACE™ far exceeds that of a simulated patient or role player.
The role of the ACE™ therefore is to give feedback on all of the above. This will ensure that the student performs the examination correctly,to the standard of the current OSCE curriculum and demonstrates safe practice. As you can see the function of the ACE™ far exceeds that of a simulated patient or role player.