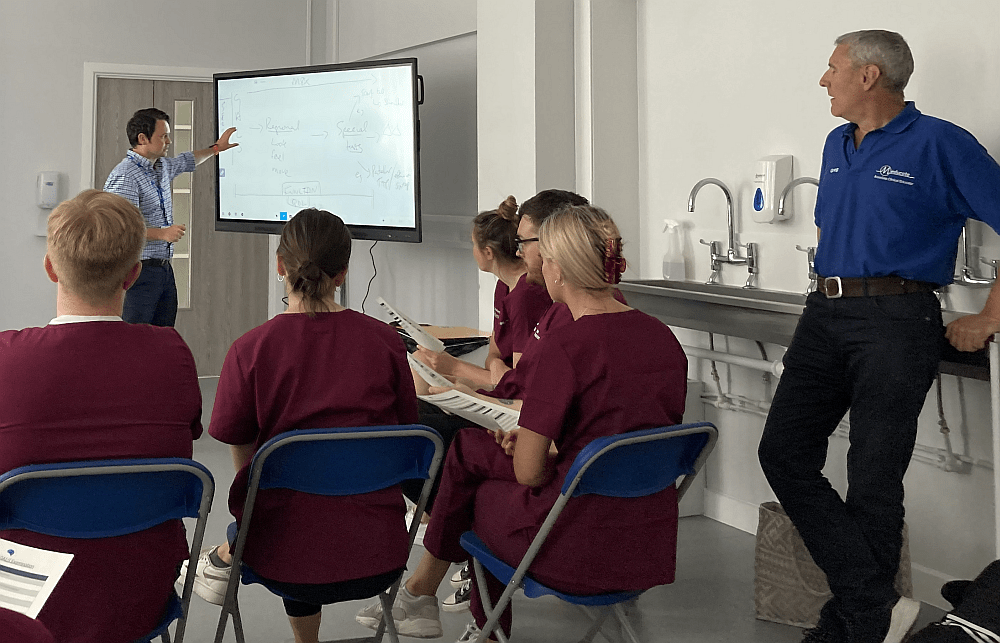
Mark and Helen of Meducate Academy listen in as Clinical Lead James Ennis teaches the finer points of systems examination.
It’s always busy at Meducate Academy and some weeks are busier than others, but what is it an ACE does? What’s a typical week in the life of an ACE? It’s a question I often get asked by students and role-players and friends alike.
To answer that question I thought I’d keep a diary of a typical week and hopefully answer those questions. It might also help those medical role-players gain some insight as to whether they want to take the next step and start training to become an ACE and take their abilities to the next level.
So let’s take a look at a typical week.
The week started as it usually does with checking emails and messages that might be left on social media. LinkedIn seems to be the best one for keeping in touch with colleagues at institutions around the country and abroad.
Once that’s out of the way, I will usually look at some scenarios and teaching sessions that may be on the timetable that week. It always pays to prepare for some of the more technical sessions we are involved in. Cranial nerves examinations, for some reason, seem to scare ACEs as much as it does the students, but because I’ve been working as an ACE for over 12 years, I don’t find this as daunting.
The week we are looking at was varied and included respiratory, cardio and a brief session on Gastro Intestinal examinations.
As the students were first-year Physician Associates, it was important that I also understood what was required of me by the clinicians. Every clinician has their way of carrying out these types of examinations, and it’s important that we, as ACEs, ensure that we are all singing from the same hymn sheet.
Experienced clinicians often take shortcuts in clinical practice when examining a patient. This is because they have many years of experience working in medicine. Students are often confused by this approach particularly because the methodology used in training is far more detailed.
My experience working as an ACE, has made me realise that students frequently get confused about this approach and what is required of them in terms of how they should examine a patient effectively, efficiently and safely.
I always use the driving test as an analogy. When we learn to drive, we have to be meticulous about every detail, and every nuance and develop the technique of driving until we have unconscious competence. Only then, once we have passed the test and thrown away the L plates do we learn to drive efficiently. Some things we needed to do to pass the driving test are no longer useful to us, so they’re discarded. It’s almost the same process as learning physical examinations. Once we have explained this to the students it becomes obvious why they have to learn a systems exam in such detail. When they have finally qualified this methodology shows its potential.
As an ACE, I always explain that my job is to guide them through the processes involved that will allow them to demonstrate in an OSCE just how competent they are examining one system at a time.
Once they move into the second year, the distinction blurs. Patients often have more than one pathology, so if a patient turns up with shortness of breath, there might be several causes. This is when the student thinks of the patient holistically and not as just one body system.
During this particular week, I had been asked to take 2nd years through a very brief, but focused, cardio and respiratory examination. This meant they had to start thinking logically and clinically about how to examine the patient, both from a respiratory and a cardiovascular perspective. Blending two systems examinations effectively is difficult. Teaching in this way is very rewarding, not just for the student but for the ACE. We also have to think about how best to teach these skills to the student.
The first-year students we taught this week were practising the Cardio examination and having to do it to the clock. As OSCEs are always timed, the students also have to deal with time pressure. A typical OSCE is 2 minutes of reading time and 8 minutes in the room with a patient and an examiner. In that 8 minutes, they only have 7 minutes to examine and 1 minute to give a management plan. The ACE needs to be aware of the acronym SBAR (Situation, Background, Assessment and Recommendations).
Working like this can be stressful for the student, and part of our role is to keep the student motivated and confident: teaching and therapy all in one.

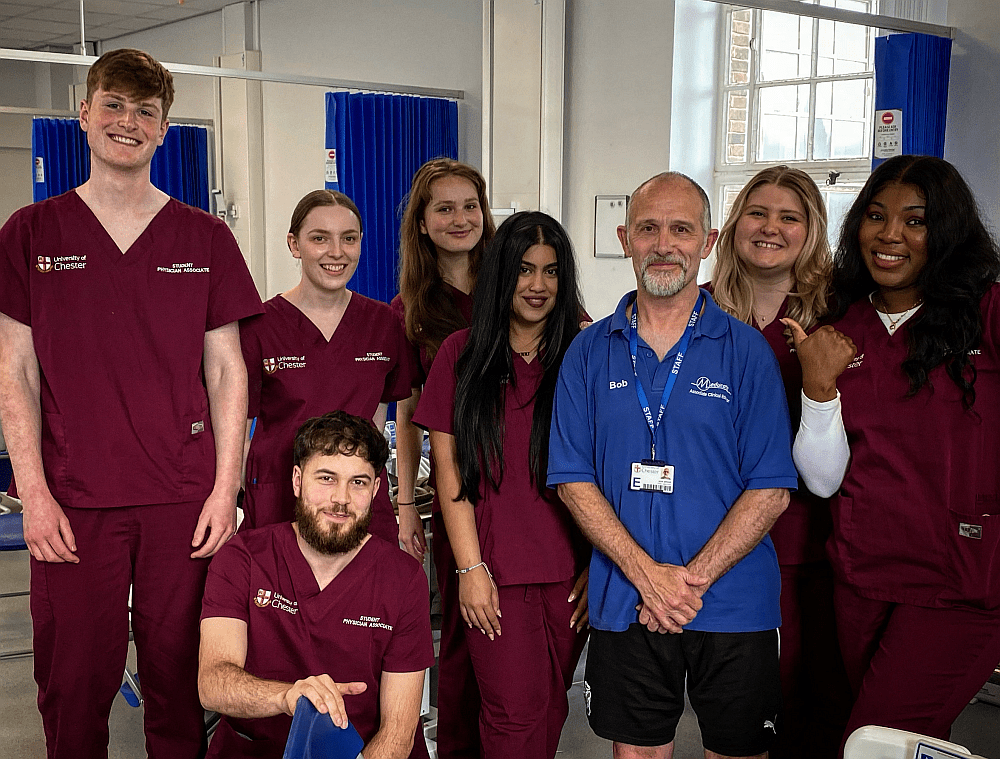
We take accreditation seriously. Prof Jim Parle looks on as ACEs demonstrate their knowledge of the hand examination
The sessions above took place over two days with Physician Associate students. Later in the week, I worked alongside GPs in collaboration with Orthopathways. A medical training company developing new software to aid GPs in diagnosing and the treatment of MSK pathologies. I was playing the role of a patient with different pathologies and then giving feedback to the GP. I worked with twenty GPs during that month, and I look forward to continuing working with them again.
The week concluded with teaching history taking and communication skills to 1st-year students. An essential skill for any health professional and particularly important for Medical Students and Physician Associates. All ACEs have to have had some training in Medical Roleplay before they can become an ACE.
The above is an example of a busy week. Sometimes it is quieter due to holidays and students going out on placement. These are the times I employ to ensure that my skill set is still high by taking advantage of reading books on the subject and looking at online resources.
I have learned to be cautious of making assumptions about what is expected of the ACE. We need to be flexible about the programmes institutions run, as their teaching methodologies can vary. Each institution has its approach to the teaching of medicine, and the ACE must be aware of these differences. ACEs must keep up to date with the latest teaching methodologies that medical schools currently employ. It pays to get hold of the teaching materials the staff use at these institutions. These will assist you when working with the students.
For those of you who might wish to embark upon this career as an ACE, get in touch with us now. Please contact: bobspour@meducateacademy.com.