My journey as An Associate Clinical Educator started way back in 1984 when I enrolled on the Drama and Theatre Arts Degree course at The University of Birmingham. It was a massive departure from my previous life back in the North of England. I was a mature student and at least ten years older than my fellow students, and the real challenge was also having two small children in tow! The course was the best thing I could have done and has changed my life immeasurably.
I would never have imagined that many years later I would work as an associate clinical educator at the same university but this time in the Medical School and not the Drama department.
After qualification I was working as an actor in TV, Film, Theatre and Motion Capture. I served a fifteen year apprenticeship as a comedian on the alternative comedy circuit through the late 80s to the early noughties as part of a double act.
It was during my time as a comedian that I was able to develop skills as an performer and spent this time persuading the audience that we were funny. Working as a live comedian is the best place to learn to deal with an audience. If you don’t get your message across, you are told to “Get Off”. Not usually as politely as that!
In the background to this I was also building my skills as a corporate educator, motivational speaker, and a Trainer of NLP (Neuro Linguistic Programming). NLP is something I continue to be involved with to the present day.

In 2009 I changed direction and applied to be a Medical Role Player with The Interactive Skills Unit (ISU) at The University of Birmingham. This required a different set of skills and as well as acting I was also expected to give feedback to the medical students after having role played various scenarios with them. A different way of working for me, and I enjoyed it immensely.
It was during a GPVTS roleplay session that the Manager of the ISU, Karen Reynolds, approached me and asked if I would be interested in working as an ACE. This was a role developed by Professor Jim Parle of The Physician Associate Programme at Birmingham. I jumped at the chance and embraced this new venture. It would shape the course of my future career working with health professionals.
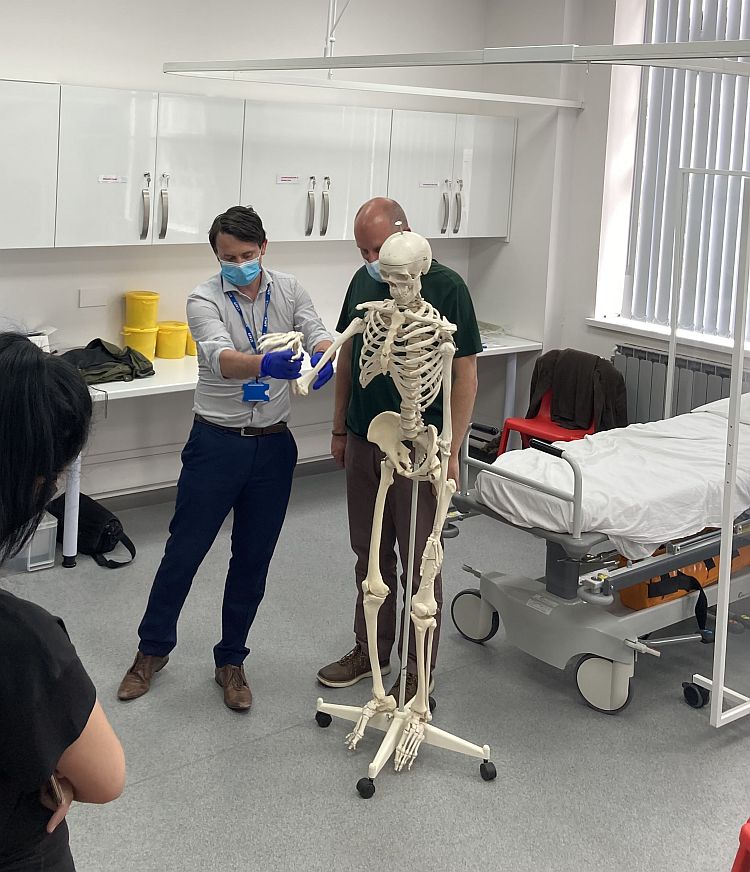
With the help of Jim Parle I embarked upon my new career as an ACE. It meant I could combine my skills as a communicator alongside my new growing knowledge of body systems examinations. Giving feedback on the students technique as well as their communication skills. I could now help the student on two levels. Having been a trained engineer in the 70s I took to the role easily, as body systems are not dissimilar to mechanical systems. I also took this approach whilst studying anatomy and physiology.
Over the next six months I bought books on body system examinations and practiced the techniques with Mark, one of the other ACEs. Together we made a formidable team and worked with The Physician Associates and their Clinical staff. The clinicians were always supportive of our efforts and always made us feel part of the team. They gave us insight into the methodology of examining the CV, respiratory, GI, cranial nerves, upper and lower limb neurology. We also helped the students’ approach to sitting the OSCEs (Objective Structured Clinical Exams). We were learning on the job and I spent many hours pouring over medical textbooks to enhance my knowledge in my own time.
In 2011 I was offered a chance to learn examinations of the musculo-skeletal systems, working for The Royal Orthopaedic Hospital (ROH). Training was carried out by Consultant Surgeon Mr Edward Davis and Consultant Physiotherapist Andy Emms. These sessions were well structured, theoretical and practical, and they guided us through the hip, knee, shoulder, spine, hand and ankle examinations in great detail along with supporting materials. This would be another string to my bow.

As time went on, I was fortunate to work with some great clinicians who were always happy to help and answer my questions. Some have even become friends as well as colleagues.
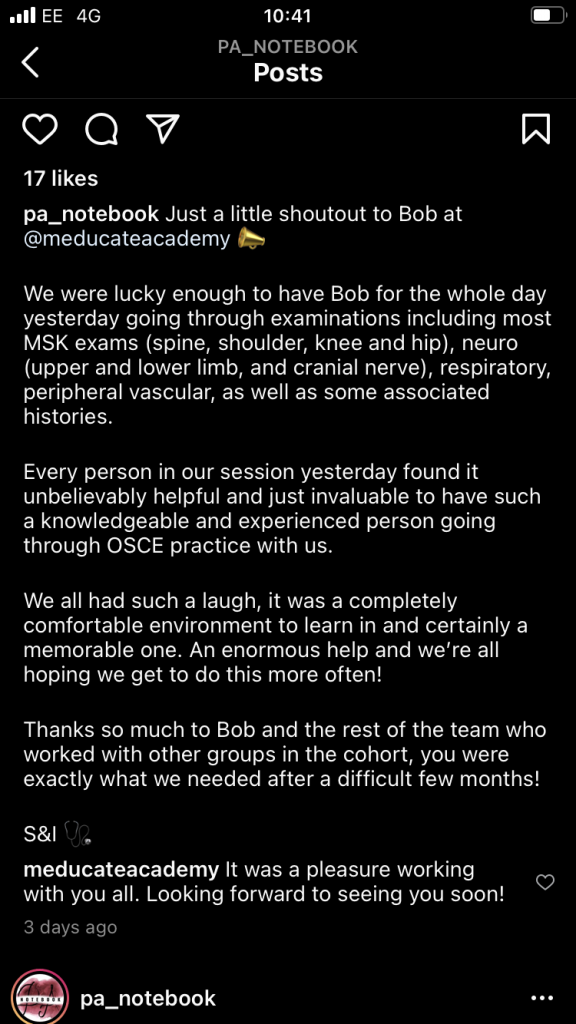
I now have the pleasure of extending my knowledge to other universities and institutions and find myself able to offer employment and training to other role players and actors wishing to embark on this amazing career.
I am also in the process of creating a course with a view to ACEs gaining accreditation for the role through one of our partners. I believe this is vitally important in maintaining high standards of teaching to the medical students. Many of the clinicians I have worked with over the years have offered their help in teaching new ACEs to the very highest level.
Who would have thought it would have come this far? It’s thanks to the people who gave me the opportunity to reach out to students and help them on their journey to becoming great clinicians.
The recent pandemic saw a downturn with employment in the field for many role players, but I was able to take up this challenge and run with it. Working in conjunction with Peter Gorman at The University of Wolverhampton and James Ennis at Chester University, we were able to teach online and take OSCEs from March 2020 right up to the present date. Thus ensuring the students had as little disruption as possible to their studies. Sadly, some universities did not embrace this way of working until much later. We were therefore ahead of the curve in adapting to the changing working environment and I was able to offer employment to some of my friends and colleagues.
It is during tough times like this that I fully realise the significance of one of my lifelong maxims:
There is no Failure. Only Feedback.
If 2020-21 was anything to go by, 2022 promises to be an exceptional year for Meducate Academy. This is how I see the future.
If you, like me, fancy a real challenge, come work with Meducate Academy and join us on the journey.